How Does Snoring Affect Your Risk of Diabetes?
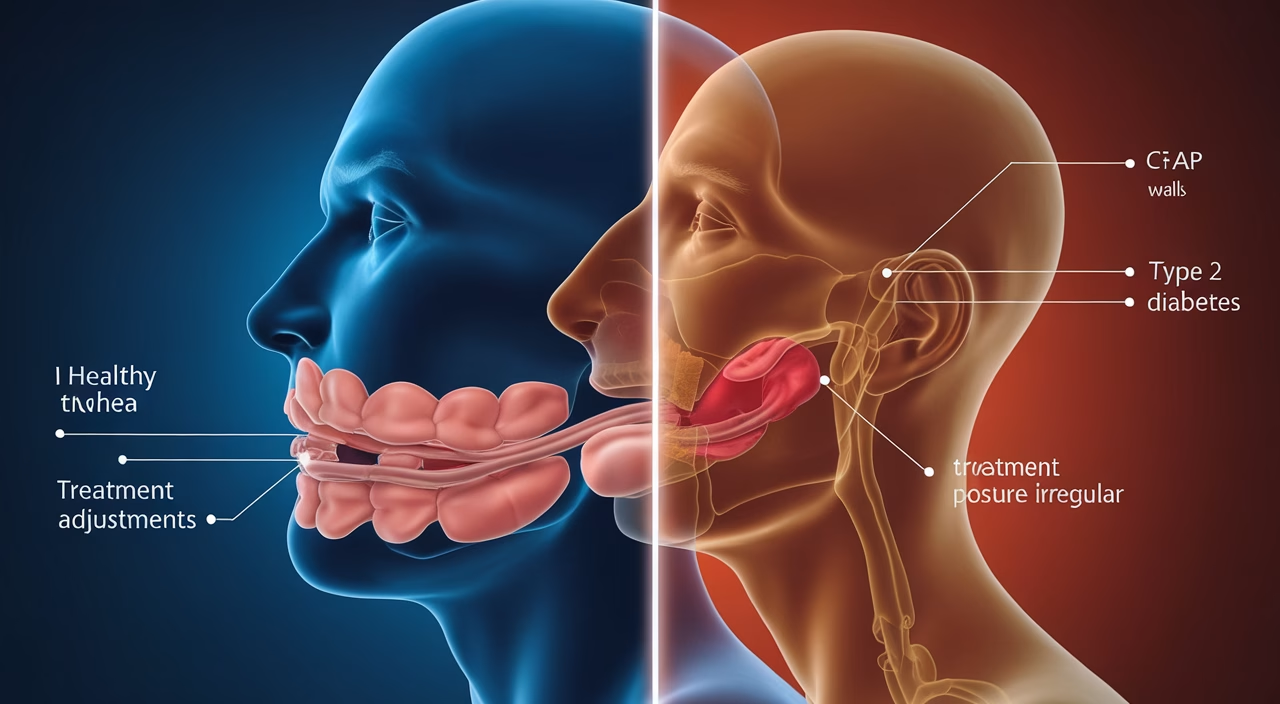
Short answer: Snoring, especially when linked to sleep apnea, can significantly disrupt your sleep architecture, leading to poor glycemic control, insulin resistance, and higher risks of developing or worsening type 2 diabetes.
TL;DR Summary
- Snoring isn’t just a nuisance — it can be an early warning sign of obstructive sleep apnea, which affects how your body manages blood sugar.
- Poor sleep quality, interrupted by snoring, negatively impacts insulin sensitivity, making it harder to regulate glucose levels.
- If you have prediabetes or type 2 diabetes, untreated snoring or sleep apnea might be silently worsening your condition.
- Solutions like weight management, CPAP treatment, and sleep hygiene can reduce snoring and improve glycemic outcomes.
- Addressing snoring can be a powerful step toward preventing diabetes complications or even delaying its onset in high-risk individuals.
Understanding the Connection Between Snoring and Diabetes
Many people view snoring as a harmless (if annoying) nighttime occurrence. But what if that noisy breathing during sleep could be one of the first signs your health is veering off track?
The relationship between snoring and diabetes might seem unrelated on the surface, but deep inside your body, the ties run surprisingly strong. When you snore — particularly if it’s due to obstructive sleep apnea — your breathing repeatedly stops and starts. Each episode triggers a drop in blood oxygen levels, followed by a stress hormone surge. This combination can sabotage your metabolism, insulin function, and even lead to insulin resistance — a stepping stone to diabetes.
Consider this: people with sleep apnea are at a 2–4 times higher risk of developing type 2 diabetes. For those already diagnosed, untreated sleep-breathing disorders can majorly disrupt their glycemic health.
We’re not just talking about restless nights. We’re talking about chronic blood sugar spikes, increased inflammation, and metabolic chaos — all influenced while you sleep. And often, the first clue is a partner nudging you to stop snoring.
The Impact of Snoring on Glycemic Health
Let’s zoom in on your body’s glucose-regulating engine — the delicate system that keeps blood sugar stable. During restful sleep, hormones like insulin and cortisol perform a balancing act. But throw in frequent snoring episodes and this harmonious process becomes disruptive to your glycemic health.
What Happens Physiologically?
When snoring coincides with sleep-disordered breathing, it triggers:
- Repeated drops in oxygen saturation
- Elevated sympathetic activity (your “fight or flight” response)
- Increased inflammatory markers like CRP and IL-6
- Insulin resistance in muscle and fat tissue
This means that over time, your cells become less responsive to insulin, forcing the pancreas to pump out even more. Eventually, the system can’t keep up — and blood sugar levels begin to climb, directly impacting your glycemic health.
Recent longitudinal studies show that untreated sleep apnea — often marked first by heavy snoring — correlates strongly with higher HbA1c levels (a long-term marker of blood glucose control).
How It Feels in Real Life
Here’s what often happens: You wake up feeling unrested, even after 8 hours in bed. You battle cravings, daytime fatigue, and see unpredictable changes in blood sugar numbers — despite eating the same meals. That’s because quality of sleep, not just quantity, affects your glycemic health more than you think.
Growing Body of Evidence
In one meta-analysis of over 30 studies, patients with severe sleep apnea had a 70% higher risk of developing type 2 diabetes than non-apneic individuals. Even those with milder snoring patterns showed early signs of impaired glucose tolerance, highlighting how snoring risk factors compound over time.
Identifying the Risk Factors: Snoring and Prediabetes
Prediabetes is the warning light on your metabolic dashboard — and snoring might be one of its most overlooked triggers or accelerators. Understanding these snoring risk factors can help you take action before diabetes develops.
Snoring Risk Factors That Raise Diabetes Risk
- Excess weight: Fat deposits around the neck restrict airflow and increase insulin resistance.
- Age and gender: Men over 40 are particularly at risk, though women catch up post-menopause.
- Poor sleep hygiene: Inconsistent sleep patterns can destabilize metabolism and worsen glycemic health.
- Family history of type 2 diabetes
- High stress levels or sedentary lifestyle
For many, snoring starts subtly but worsens with each gained pound. If you’re already in the prediabetic zone, it’s worth watching this overlap closely — especially if glycated hemoglobin (HbA1c) or fasting glucose numbers are on the rise despite lifestyle changes.
Real Example
One patient we worked with presented with mild snoring, borderline glucose levels, but no overt signs of diabetes. A sleep study revealed moderate sleep apnea. After CPAP therapy and weight loss, both his snoring and blood glucose normalized, averting a slide into diabetes and dramatically improving his glycemic health.
Managing Snoring to Improve Diabetes Control
Here’s the good news: snoring isn’t a life sentence. There are actionable strategies you can take today that not only quiet your nights but may also lower your risk of diabetes or improve its management.
What Works Best for Snoring and Diabetes?
- Weight Management: Even a 10% reduction in body weight can drastically lower both snoring and insulin resistance while improving glycemic health.
- Positional Therapy: Sleeping on your side often reduces airway obstruction and snoring episodes.
- CPAP Therapy: The gold standard for treating sleep apnea — this can improve insulin sensitivity and reduce HbA1c in as little as 3 months.
- Sleep Hygiene Practices: Regular sleep schedules, dark bedrooms, and limiting screen time before bed help stabilize blood sugar indirectly by enhancing sleep quality.
Cost Guide: Managing Snoring-Related Sleep Disruption
| Solution | Low Range | Mid Range | High Range |
|---|---|---|---|
| Sleep Study | $150 | $400 | $1,200+ |
| CPAP Machine | $300 | $600 | $1,000 |
| POS Therapy Devices | $50 | $150 | $500 |
| Consultation & Follow-Up | $100 | $300 | $700 |
Effective Solutions for Snorers with Diabetes
So what should you do if you’re experiencing both snoring and blood sugar issues? Combine medical, behavioral, and lifestyle measures tailored to your specific snoring risk factors and glycemic health needs.
Top Snoring Solutions for Diabetes Patients
- Device-based therapies: CPAP, oral appliances, and nasal expanders are particularly effective when snoring is diagnosed as related to sleep apnea.
- Diet and Exercise: Plant-forward, whole-food-based diets and 30 minutes of movement per day enhance both weight loss and insulin sensitivity — reducing snoring severity and improving glycemic health.
- Continuous Monitoring: Keep a symptom-sleep log, use a CGM if diabetic, and track progress on both snoring and diabetes markers.
- Seek professional help: An overnight sleep study remains the best way to diagnose conditions like sleep apnea that impact both snoring and diabetes risk.
Final Thought
Snoring may seem like an innocent annoyance, but its impact runs deeper — particularly if you’re navigating the waters of prediabetes or an existing diabetes diagnosis. Underestimating snoring means missing a crucial piece of your metabolic puzzle.
By addressing snoring and its risk factors early, you not only regain restful sleep but also take back control over your glycemic health, insulin response, and long-term well-being. Don’t dismiss loud nights as “just snoring.” Sometimes, it’s your body whispering that something bigger needs attention.
Frequently Asked Questions
- Will treating sleep apnea help with diabetes?
Yes. Treating sleep apnea, especially with CPAP therapy, often leads to improved insulin sensitivity and better blood sugar control, significantly enhancing your glycemic health. - How does snoring affect blood sugar levels?
Snoring can disrupt sleep quality and interfere with hormonal balance, leading to insulin resistance and higher glucose levels over time, compromising your overall glycemic health. - Can snoring lead to diabetes complications?
Yes. Unaddressed sleep issues worsen glycemic control, potentially increasing diabetic complications like neuropathy, nephropathy, and cardiovascular risk. - Is there a way to prevent diabetes by improving sleep?
Improving sleep quality — including treating snoring — can enhance insulin function and reduce the risk of developing diabetes in predisposed individuals by addressing key snoring risk factors. - What’s the link between snoring and insulin resistance?
Interrupted sleep breathing patterns result in stress hormone spikes, which make cells less responsive to insulin, a condition called insulin resistance that directly impacts glycemic health. - Are snoring solutions safe for people with diabetes?
Most treatments like CPAP, oral appliances, and lifestyle interventions are safe and beneficial for diabetic individuals, often improving both snoring and glycemic health when supervised by a healthcare provider. - When should I get a sleep study?
If you experience loud snoring, daytime fatigue, or poor glucose control despite other efforts, it’s time to get assessed — especially if you have multiple snoring risk factors.